Cite as: Oxman AD, Chalmers I, Dahlgren A (2022). Key Concepts for Informed Health Choices: 1.3 Seemingly logical assumptions about treatments can be misleading. James Lind Library (www.jameslindlibrary.org).
© Andy Oxman, Centre for Epidemic Interventions Research, Norwegian Institute of Public Health, Norway. Email: oxman@online.no
This is the third of four essays in this series explaining key concepts that can help you avoid being misled by claims that have an untrustworthy basis. In this essay, we explain five seemingly logical assumptions about treatments that can be misleading. These assume that:
- treatment is needed,
- more treatment is better,
- a treatment is helpful or safe based on how widely used it is or has been,
- a treatment is better based on how new or technologically impressive it is, or
- earlier detection of ‘disease’ is better.
The basis for these concepts is described elsewhere [Oxman 2022].
Do not assume that treatment is needed.
Effective treatments can prevent health problems and premature death and improve the quality of life. However, nature is a great healer and people often recover from illness without treatment. Likewise, some health problems may get worse despite treatment, or treatment may even make things worse. Not using a treatment is not the same as “no treatment”. Waiting to see what happens (“letting nature take its course”), with or without treating symptoms such as pain, is a treatment option.
Sore throats are an example of an illness that gets better without treatment. Sore throats caused by bacteria (strep throat) have been treated with antibiotics primarily to prevent rheumatic fever. Rheumatic fever still occurs in some parts of the world, but it is very rare in many parts of the world. In those parts of the world antibiotics are used primarily to promote faster recovery. Antibiotics have a modest effect on recovery in the first few days, but after seven days, 90% of patients are symptom-free with or without antibiotics [Spinks 2013]. Moreover, antibiotics have adverse effects, including diarrhoea and rash, and widespread use of antibiotics contributes to antibiotic resistance.
Do not assume that more treatment is better.
Increasing the dose or amount of a treatment (e.g., how many vitamin pills you take) can increase harms without increasing beneficial effects.
For example, iron deficiency is an important cause of anaemia and a major contributor to the global burden of disease [Pasricha 2021]. Iron supplements are effective for preventing and treating iron deficiency anaemia. However, iron supplements can injure the upper gastrointestinal tract and cause nausea, vomiting, discomfort, diarrhoea, and constipation – and higher doses of iron increase the number and severity of adverse effects [Cancelo-Hidalgo 2013].
More aggressive treatment can also increase harms without increasing benefits. For example, radical mastectomy entails removing the breast tissue along with the nipple, lymph nodes in the armpit, and chest wall muscles underneath the breast. This was standard care for breast cancer surgery for almost a century. But in the 1980s, fair comparisons found that a lumpectomy was an equally effective option that was far less extensive and easier on the patient. It removed the tumour, but not the breast itself [Cotlar 2003].
Do not assume that a treatment is helpful or safe based on how widely used it is or has been.
Treatments that have not been properly evaluated but are widely used or have been used for a long time are often assumed to work. Sometimes, however, they may be unsafe or of doubtful benefit.
Bloodletting, taking blood from a patient to prevent or cure illness, was the most common procedure performed by physicians and surgeons for almost two thousand years [Science Museum 2009]. As late as 1923, it was recommended in Principles and the Practice of Medicine [Stewart 2019]. In addition to not being helpful, bloodletting was not safe. People were killed from blood loss, including George Washington, the first president of the U.S. [Morens 1999]. It could also lead to severe or even fatal infections.
Medicine to reduce heart rhythm abnormalities is a more recent example of a widely used treatment that was deadly. Because heart rhythm abnormalities are associated with an increased risk of early death after a heart attack, it was believed that medicines that reduced these abnormalities would also reduce early deaths. These medicines were used for many years before it was discovered that they increase the risk of sudden death. It has been estimated that, at the peak of their use in the late 1980s, they may have been killing as many as 70,000 people every year in the U.S. alone [Moore 1995].
Do not assume that a treatment is better based on how new or technologically impressive it is.
New treatments can be assumed to be better simply because they are new, more expensive, or technologically impressive. However, on average, they are only very slightly likely to be better than other available treatments. Some side effects of treatments, for example, take time to appear, and without long term follow-up it may not be possible to know whether they will appear.
Vioxx (rofecoxib) was a new non‐steroidal anti‐inflammatory drug (NSAID) prescribed to decrease pain and inflammation in arthritis and acute pain in adults. Fair comparisons showed that more people who took Vioxx for eight weeks had relief from arthritis symptoms than people who took a ‘sugar pill’ or placebo, and that it worked just as well as Naprosyn [Garner 2005]. Vioxx was approved by the U.S. Federal Drug Administration (FDA) in 1999. The producer of Vioxx spent $161 million advertising Vioxx with advertisements like this:
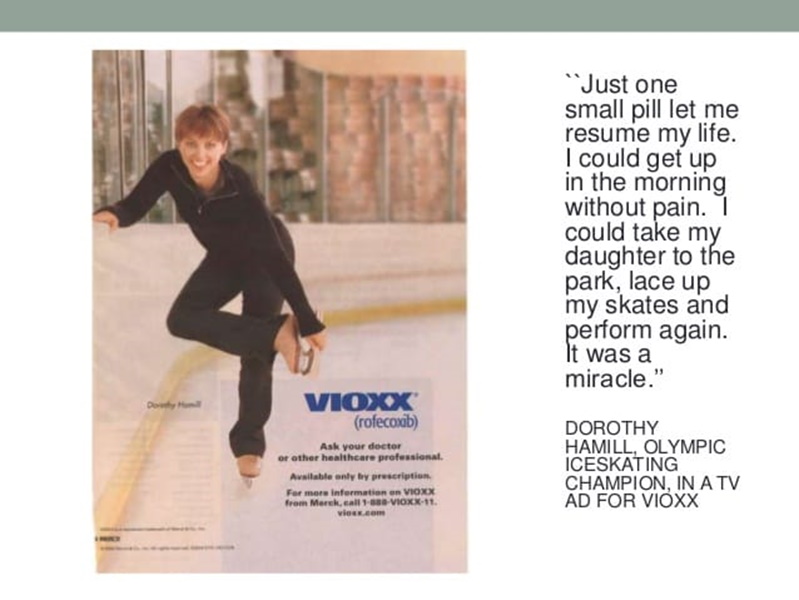
However, Vioxx was withdrawn from the market in 2004 after it was shown that long-term use increased the risk of heart attack and stroke.
Do not assume that earlier detection of ‘disease’ is better.
People often assume that early detection of disease and ‘treating’ people who are at statistical risk of disease lead to better outcomes. However, screening people to detect disease or treating people at statistical risk of disease is only helpful if two conditions are met. First, there must be an effective treatment. Second, people who are treated before the disease becomes apparent must do better than people who are treated after the disease becomes apparent. Screening and treating people at statistical risk of a disease can lead to overdiagnosis and overtreatment. Screening tests can be inaccurate (e.g., misclassifying people who do not have a disease as if they do have the disease). Screening or treating a statistical risk factor as if it is a ‘disease’ can also cause harm by labelling people as being sick when they are not, and because of side effects of the tests and treatments.
Screening for phenylketonuria (PKU) is an example of early detection of disease that is better than late detection. PKU is a rare inherited disorder. People with PKU cannot metabolise phenylalanine. Untreated, PKU results in severe intellectual disability, epilepsy, and behavioural problems. PKU can be detected in newborn babies with a drop of blood. Treatment includes a special diet and regular blood tests. With early diagnosis and treatment, most children with PKU can live healthy lives [van Wegberg 2017].
Screening women without symptoms for ovarian cancer is an example of early detection that does more harm than good. In randomized trials with nearly 300,000 women, there was not an important difference in the numbers of women who died from ovarian cancer between women who were screened and those who were not [Henderson 2018]. Harms of screening included surgery (with major surgical complications) in women found to not have cancer.
Implications
- Always consider the usual course of a health problem when considering treatments other than waiting to see what happens. Sometimes treatment is not needed and may even make things worse.
- If a treatment is believed to be beneficial, do not assume that more of it is better.
- Do not assume that treatments are beneficial or safe simply because they are widely used or have been used for a long time unless this has been shown in systematic reviews of fair comparisons of treatments.
- Do not assume that a treatment is better or safer simply because it is new, brand-named, expensive, or technologically impressive.
- Do not assume that early detection of disease is worthwhile if it has not been assessed in systematic reviews of fair comparisons between people who were screened and people who were not screened.
< Previous Essay | Next Essay >
This James Lind Library Essay has been republished in the Journal of the Royal Society of Medicine 2022;115:448-450. Print PDF
References
Cancelo-Hidalgo MJ, Castelo-Branco C, Palacios S, Haya-Palazuelos J, Ciria-Recasens M, Manasanch J, et al. Tolerability of different oral iron supplements: a systematic review. Curr Med Res Opin. 2013;29(4):291-303. https://doi.org/10.1185/03007995.2012.761599
Cotlar AM, Dubose JJ, Rose DM. History of surgery for breast cancer: radical to the sublime. Curr Surg. 2003;60(3):329-37. https://doi.org/10.1016/s0149-7944(02)00777-8
Garner SE, Fidan D, Frankish RR, Judd M, Towheed T, Tugwell P, et al. Rofecoxib for rheumatoid arthritis. Cochrane Database Syst Rev. 2005(1):CD003685. https://doi.org//10.1002/14651858.CD003685.pub2
Henderson JT, Webber EM, Sawaya GF. Screening for ovarian cancer: an updated evidence reviewfor the U.S. Preventive Services Task Force. Rockville (MD): Agency for Healthcare Research and Quality (US); 2018. http://www.ncbi.nlm.nih.gov/books/nbk493399/
Moore TJ. Deadly Medicine: Why Tens of Thousands of Heart Patients Died in America’s Worst Drug Disaster. New York: Simon & Schuster; 1995.
Morens DM. Death of a president. N Engl J Med. 1999;341(24):1845-9. https://doi.org/10.1056/nejm199912093412413
Oxman AD, Chalmers I, Dahlgren A, Informed Health Choices Group. Key Concepts for Informed Health Choices: a framework for enabling people to think critically about health claims (Version 2022). IHC Working Paper. 2022. http://doi.org/10.5281/zenodo.6611932
Pasricha S-R, Tye-Din J, Muckenthaler MU, Swinkels DW. Iron deficiency. Lancet. 2021;397(10270):233-48. https://doi.org/10.1016/S0140-6736(20)32594-0
Science Museum. Bloodletting, 2009. https://www.sciencemuseum.org.uk/objects-and-stories/medicine/blood#bloodletting
Spinks A, Glasziou PP, Del Mar CB. Antibiotics for sore throat. Cochrane Database Syst Rev. 2013;2013(11):Cd000023. https://doi.org/10.1002/14651858.cd000023.pub4
Stewart O. Bloodletting: a brief historical perspective and modern medical applications. Clinical Correlations, October. 2019;31. https://www.clinicalcorrelations.org/2019/10/31/bloodletting-a-brief-historical-perspective-and-modern-medical-applications/
van Wegberg AMJ, MacDonald A, Ahring K, Bélanger-Quintana A, Blau N, Bosch AM, et al. The complete European guidelines on phenylketonuria: diagnosis and treatment. Orphanet J Rare Dis. 2017;12(1):162. https://doi.org/10.1186/s13023-017-0685-2
